In recent years, Deep Brain Stimulation has been gaining traction in the scientific community because of its perceived potential to become an effective treatment for addiction. This paper argues that Deep Brain Stimulation is indeed an effective treatment for humans with addiction problems for three primary reasons. First, Deep Brain Stimulation’s mechanism has been proven to successfully aid in correcting brain dysfunction by targeting specific parts of the organ, and the same mechanism can be replicated to treat addiction. Second, Deep Brain Stimulation has been seen in several cases to treat addictive behaviors in various patient groups. Lastly, Deep Brain Stimulation is a form of treatment that is relatively easy for patients to undergo, which means that the treatment can maximize its potential and take full effect on the patient.
Deep Brain Stimulation’s Mechanism
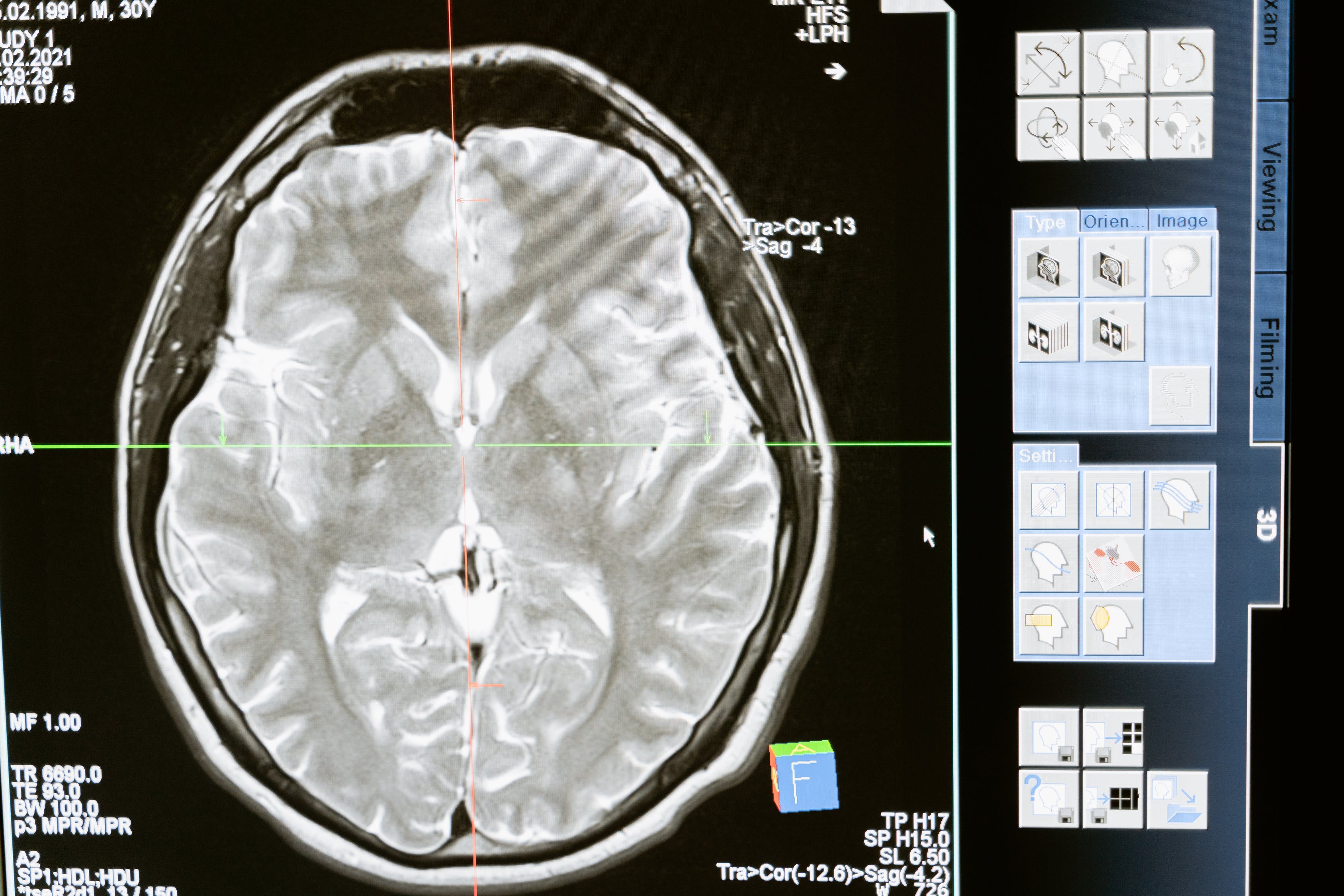
Deep Brain Stimulation is a surgical process where one or more electrodes are implanted into specific areas of the brain so that these electrodes can correct abnormal patterns of neural signaling in that area (Hickey & Stacy, 2016). It is precisely for this reason that the treatment is used for Parkinson’s Disease, a disorder where the patient gradually loses control over movements, gait, and balance. In the latter stages of the disease, patients can lose control of their motor abilities far beyond than what medication can sufficiently address, and it is in these scenarios where Deep Brain Stimulation has proven successful. For example, a study conducted in Germany and Austria with 156 Parkinson’s Disease patients who underwent bilateral Deep Brain Stimulation revealed that, after 6 months of treatment, Deep Brain Stimulation has given them significantly better quality of life measures and motor scores in comparison to a control group who did not receive the same treatment. Additionally, dyskinesia – a condition characterized by abnormal voluntary movements – reduced by 54% more in the patient group that received Deep Brain Stimulation treatment than those in the group that received only medication (Hickey & Stacy, 2016).
With its success in treating Parkinson’s Disease, it has been surmised that the same mechanism can be applied to treating in addiction in humans. Many studies concerning treating addiction using Deep Brain Stimulation have been conducted on animals since the early 2000s, and the results have been promising: by targeting another part of the brain – the nucleus accumbens – Deep Brain Stimulation was able to reduce drug-seeking behavior (Wang et Al, 2018). By correcting abnormal patterns of neural signaling in this area, Deep Brain Stimulation was able to improve the neuroplastic changes that the mesolimbic reward pathway undergoes, which, in the context of drug addiction, typically leads to a subdued functioning of the prefrontal cortex and decreased impulse control (Wang et al, 2018).
Deep Brain Stimulation’s Impact on Treating Addictive Behaviors
While Deep Brain Stimulation has been showing promise via animal studies, it has also been shown to bear significant results in treating addictive behaviors in humans, particularly in various patient groups. Because of Deep Brain Stimulation’s success with Parkinson’s Disease patients, this form of treatment has been expanded to accommodate several other disorders such as anxiety disorders, obsessive-compulsive disorders, and Tourette’s syndrome – and despite the fact that Deep Brain Stimulation was used primarily as treatment for these diseases, patients who underwent this treatment have also shown signs of “improvements in alcohol misuse, heroin use, and cigarette addiction” (Zullino et al, 2016). For example, a study conducted by Kuhn et al (2007) revealed that a 54-year-old patient they studied with severe anxiety disorder and who underwent Deep Brain Stimulation for treatment, focusing on the nucleaus accumbens, experienced a decrease in the patient’s alcohol dependency, which was comorbid with anxiety disorder.
Additionally, patients who are primarily treated for addiction have shown a reduction in cravings and tobacco consumption as well as increased abstinence (Zullino et al, 2016). A study conducted by Voges et al (2013) found that in the five patients with severe alcohol addiction who underwent Deep Brain Stimulation, all patients experienced “significant and ongoing improvement of craving” (Voges et al, 2013). In fact, two patients from the cohort went on for four years completely abstinent as well.
Deep Brain Stimulation’s Delivery
A pre-requisite for a form of treatment to be effective is for to patient who needs it to be a willing participant in completing the treatment, however one of the key challenges with treating addiction is in fact in this arena. Studies have shown that one challenge in effectively treating addiction in patients is the high attrition rate – as cited by Palmer et al (2009), attrition rates for substance abuse treatment programs can reach up to 30% in the first month, and drop-outs prior to three months can reach up 50% or more, despite the fact that three months of treatment is “considered to be the minimum to see symptom improvement” (Palmer et al, 2009).
High attrition rates prevent patients from maximizing the benefits of addiction treatment, thus rendering the treatment ineffective. Meanwhile, features of Deep Brain Stimulation can potentially render it a form of treatment that may be effective – if not more so – not only because of the medically proven benefits it possesses, but also because of the fact that the way its designed allows for patients to fully maximize its effectiveness. Deep Brain Stimulation does not rely on patient compliance, and thus attrition rates do not negatively impact its effectiveness in patients (Huber, 2018). Additionally, patients may also be more inclined to use Deep Brain Stimulation as a form of treatment because of its non-invasive and reversible nature, further lessening risk of attrition. Deep Brain Stimulation devices can be turned off at any time and can also be taken out of the body. Being able to stop treatment when adverse effects are occurring is crucial especially in light of addiction treatment – by being removable and non-invasive, Deep Brain Simulation prevents further damage to the body when the body rejects the implant or if infection occurs (Heinze, 2009; Trafton, 2017). Its removable nature also allows patients to still be eligible for other forms of treatments that might be more suitable for their context (University of Michigan Neurosciences, 2015), making this form of treatment attractive for patients struggling with addiction.
Counterarguments and Rebuttals
One counterargument to Deep Brain Stimulation’s effectiveness is the safety of the treatment in treating addiction in humans. Carter et al (2011) posit that “1-2% f patients who undergo Deep Brain Stimulation for Parkinson’s Disease suffer major adverse surgical outcomes like intra-cerebral hemorrhages.” In addition, says Carter et al (2011), Deep Brain Stimulation can cause serious infection, thereby producing cognitive, behavioral, and emotional dysfunction such as walking disturbances and impulsivity.
A rebuttal to this argument against Deep Brain Stimulation, however, comes also in the form of a proposal from Carter et al (2011). A solution that can be used to address this ethical issue is to set guidelines as to when, how, and for whom Deep Brain Stimulation should be used as a way to treat addiction. Carter et al (2011) outline 11 minimum ethical requirements for trials of Deep Brain Stimulation for Addiction, which include the following:
“Participant requirements:
1. Severe dependence that causes significant personal harm
2. Demonstration of treatment refractoriness
3. Access to all existing treatment provided to the highest standard
4. Capacity to consent to participate in research
5. Awareness of the risks of operation, the uncertain and limited benefits, as well as post-operative requirements (e.g. programming, battery replacement)
6. Participation that is free from coercion
Treatment and researcher requirements:
7. Motivation of the medical team to treat a medical illness and not as a form of extrajudicial punishment
8. Provision of psychosocial support post-DBS
9. Commitment of the research group to subsequent maintenance of the device
10. Performed in appropriately resourced clinics with qualified staff
11. Balanced publishing of research results, including negative results” (Carter et al, 2011).
Conclusion
Deep Brain Stimulation has shown a lot of promise in terms of being an effective treatment program for humans struggling with addiction. Its low risk and high effectiveness make it a well-accepted treatment for patients with addiction. However, the ethical issues surrounding this treatment may prevent itself from being a form of treatment that physicians will readily use or resort to. It would perhaps greatly aid physicians and researchers alike if there existed a set of fixed and accredited guidelines regarding the use of Deep Brain Stimulation on patients struggling with addiction.
REFERENCES:
Carter et al. (2011). Ethical Issues Raised by Proposals to Treat Addiction Using Deep Brain Stimulation. Neuroethics 4(2), pp. 129-142.
Heinze, H. (2009). Counteracting incentive sensitization in severe alcohol dependence using deep brain stimulation of the nucleus accumbens: Clinical and basic science aspects. Frontiers in Human Neuroscience 3, p. 22.
Hickey, P. and Stacy, M. (2016). Deep Brain Stimulation: A Paradigm Shifting Approach to Treat Parkinson’s Disease. Frontiers In Neuroscience 10(173). doi:10.3389/fnins.2016.00173
Huber, J. (2018 August 13). Deep brain stimulation might benefit those with severe alcoholism, preliminary studies show. Retrieved from: https://scopeblog.stanford.edu/2018/08/13/deep-brain-stimulation-might-benefit-those-with-severe-alcoholism-preliminary-studies-show/
Kuhn, J. et al (2007). Remission of alcohol dependency following deep brain stimulation of the nucleaus accumbens: valuable therapeutic implications? The Journal of Neurosurgeon Psychiatry 78(10), pp. 1152-1153
Palmer, R. et al. (2009). Substance abuse treatment drop-out from client and clinician perspectives. Substance Use and Misuse 44(7), pp. 1021-1038.
Trafton, A. (2017, June 1). A non-invasive method for deep brain stimulation. Retrieved October 24, 2018, from: http://news.mit.edu/2017/noninvasive-method-deep-brain-stimulation-07601
University of Michigan Neurosciences. (2015 January 15). Frequently Asked Questions: Deep Brain Stimulation. Retrieved October 24, 2018, from: http://www.uofmhealth.org/conditions-treatment/frequently-asked-questions-deep-brain-stimulation
Voges, J. et al. (2013). Deep brain stimulation surgery for alcohol addiction. World Neurosurgery 80(3), pp. 21-31
Wang, TR et al. (2018). Deep brain stimulation for the treatment of drug addiction. Neurosurgery Focus 45(2). doi: 10.3171/2018.5.FOCUS18163.
Zullino DF, Thorens G, Krack P. (2016). Deep Brain Stimulation as a Treatment for Addictions: Could Impulsivity be the Therapeutic Target? Acta Psychopathology 2(39). doi: 10.4172/2469-6676.100065